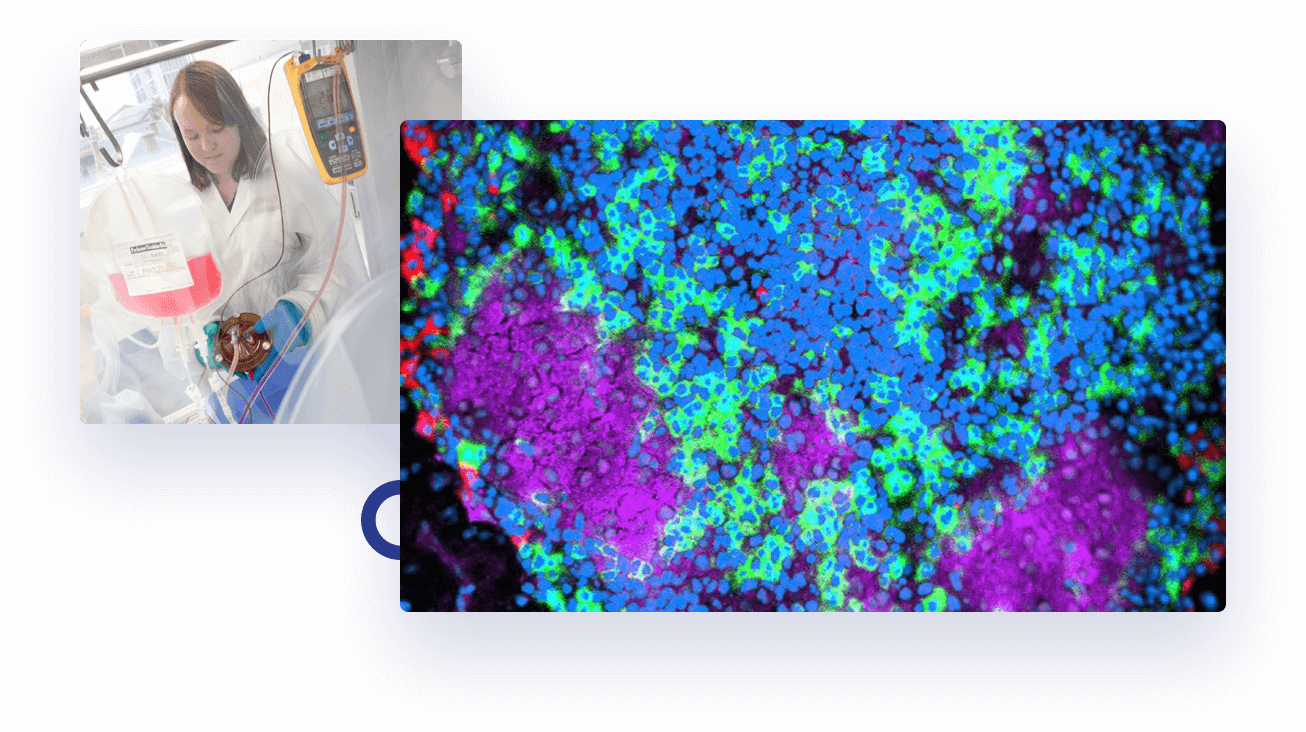
Type 1 diabetes is an autoimmune condition where, for unknown reasons, the immune system attacks the ‘beta’ cells of the pancreas that make insulin. Without insulin, blood glucose becomes dangerously high.
There are three distinct stages in the development of type 1 diabetes:
- The immune system attacks the insulin-producing beta cells in the pancreas. Blood sugar levels are normal, but autoantibodies can be detected in the blood. There are no symptoms.
- Autoantibodies are present in the blood. Blood sugar levels are out of normal range. There are no symptoms.
- The immune system has killed large numbers of beta cells. Autoantibodies are present in the blood. Blood sugar levels are abnormal, causing symptoms of thirst, weight loss and frequent urination. Insulin injections are required to control blood sugar.
A simple blood test can identify type 1 diabetes in the earliest stages; many years before irreversible damage occurs.
Recent research has identified immunotherapies that suppress this immune attack and preserve beta cells, thereby delaying or decreasing the need for insulin injections.
Testing newer immunotherapies, alone or in combination with proven ones, is a logical next step towards prevention and cure of type 1 diabetes.
Each clinical trial helps us understand who responds to immunotherapy, why they respond and what dose is optimal.
ATIC aims to work with the type 1 diabetes community to develop safe and effective immunotherapy that can be incorporated into routine clinical care. By addressing the root cause of type 1 diabetes – autoimmunity – immunotherapy promises to decrease the burden of insulin therapy and improve the lives of thousands of Australians living with the disease.
The recent success of the BANDIT trial, gives hope that immunotherapy treatment may soon provide an alternative to insulin treatment for type 1 diabetes.
Page last updated: 9 October 2024